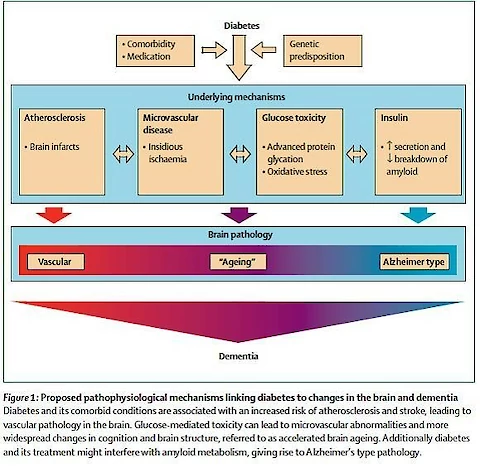
Cognitive impairment in this sense is often not easily recognized – since there is generally little or no memory problems, but rather impairment in other functions, such as executive function. This is the part of the brain associated with planning, decision making, judgement and behaviour. An unrelated and much less common form of dementia – fronto-temporal dementia also affects executive function, but this is a different process.
The implications of executive dysfunction and cognitive impairment in people suffering from diabetes can be quite profound. Consider that the objectives of health care in patients with diabetes are to minimise progression of the disease, and prevent complications. The mechanisms by which this is achieved is to follow lifestyle guidelines for diet and exercise, adhere to medication regimes and to attend check-ups and therapy with health care providers. All of these activities can be sub-optimal in someone with cognitive impairment and executive dysfunction. For people living alone without family and friends to help support their health care, this can mean increased risk of an acute event – eg. stroke, or further gradual decline in their disease process, all of which leads to increased risk of dementia.
Putting all this into context – there is a huge challenge for the health care system and for policy makers. Not only will there be a relentless and relatively rapid increase in demand for services, we must continually look at ways to try and halt or reverse these trends. This is perhaps the major problem, since it has been well known for many decades what we should be doing, but putting this into practice appears beyond our scope at present. We know for example, that type 2 diabetes can be controlled and even reversed by adopting a healthy diet and following guidelines for an active lifestyle.
Experts disagree about some of the details, and even some of the basics, but all would agree that the current Standard American Diet (appropriately referred to by its acronym SAD) which consists of a large proportion of processed food, high in refined carbohydrates, added sugar, fats and salt, and low in whole foods, combined with lack of regular exercise is the prime culprit. We know also that lower socio-economic groups are at increased risk of heading down this pathway, and these are also the groups who can least afford health care now, and will be least able to afford the cost of home care and other support that goes with a diagnosis of dementia. Those without family support face a bleak future.
While medications and treatment options continue to be developed, it is this fundamental lifestyle problem which is driving the increase in diabetes, and consequently dementia. Options to promoting healthy food choices and lifestyles are attempted, but discouraging unhealthy eating by increasing taxes on sugar, processed and fast food seem to be off the agenda, despite many public health experts arguing for this for many years. In which case we are heading inexorably to the grim scenario described above.
References
Bello-Chavolla et al Pathophysiological mechanisms linking type 2 diabetes and dementia: Review of evidence from clinical, translational and epidemiological research. Curr Diabetes Rev. 2019 Jan 15. doi: 10.2174/1573399815666190129155654. [Epub ahead of print]
Biessels et al. Risk of dementia in diabetes mellitus: a systematic review
The Lancet Neurology – Volume 5, Issue 1, January 2006, Pages 64-74 https://doi.org/10.1016/S1474-4422(05)70284-2
Dybjer et al. Pre-diabetes and diabetes are independently associated with adverse cognitive test results: a cross-sectional, population-based study BMC Endocr Disord. 2018; 18: 91. Published online 2018 Dec 4. doi: 10.1186/s12902-018-0318-3
Jansen van Vuren et al. Prospective associations between cardiac stress, glucose dysregulation and executive cognitive function in Black men: The Sympathetic activity and Ambulatory Blood Pressure in Africans study First Published December 17, 2018 Research Article Diabetes & Vascular Disease Research 1-8 https://doi.org/10.1177/1479164118816221
Janssen et al. HbA1c, Insulin Resistance, and β-Cell Function in Relation to Cognitive Function in Type 2 Diabetes: The CAROLINA Cognition Substudy. Diabetes Care. 2018 Nov 19. pii: dc180914. doi: 10.2337/dc18-0914. [Epub ahead of print]
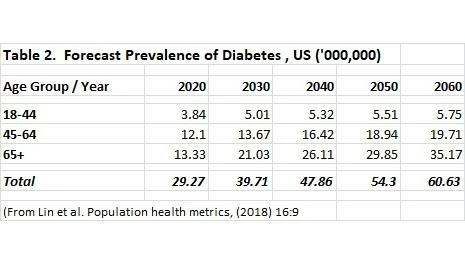
Lin et al. Projection of the future diabetes burden in the United States through 2060
Population Health Metrics 2018 16:9 https://doi.org/10.1186/s12963-018-0166-4
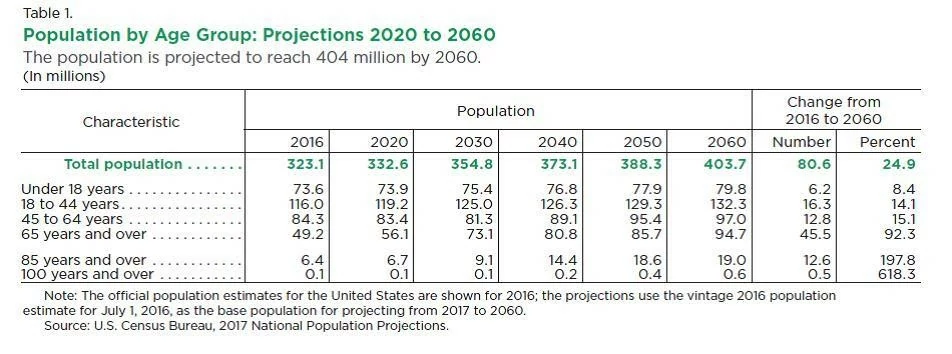
Vespa et al., Demographic Turning Points for the United States: Population Projections for 2020 to 2060 Current Population Reports, P25-1144, U.S. Census Bureau, Washington, DC, 2018.
Matthews et al. Racial and ethnic estimates of Alzheimer’s disease and related dementias in the United States (2015–2060) in adults aged over 65 years Alzheimer’s & Dementia 15 (2019) 17-24
Rowley et al. Diabetes 2030: Insights from Yesterday, Today, and Future Trends.
Popul Health Manag. 2017 Feb;20(1):6-12. doi: 10.1089/pop.2015.0181. Epub 2016 Apr 28.